Spring 2021
Research: Cannabis and Sickle Cell Disease
A recent study shows promise for patients suffering from chronic pain due to this genetic condition.
As more patients turn to cannabis to treat chronic pain conditions, research on its safety has become more vital than ever before. A recent clinical trial co-led by University of California, Irvine researcher Kalpna Gupta, PhD, and Donald Abrams, MD, of University of California, San Francisco showed that cannabis appears to be a safe and potentially effective treatment for the chronic pain suffered by those with sickle cell disease (SCD). However, a larger trial is needed to determine statistically significant differences for the effect of vaporized cannabis on pain in SCD. This is especially important given that opioids were previously the primary treatment for pain for this disease.
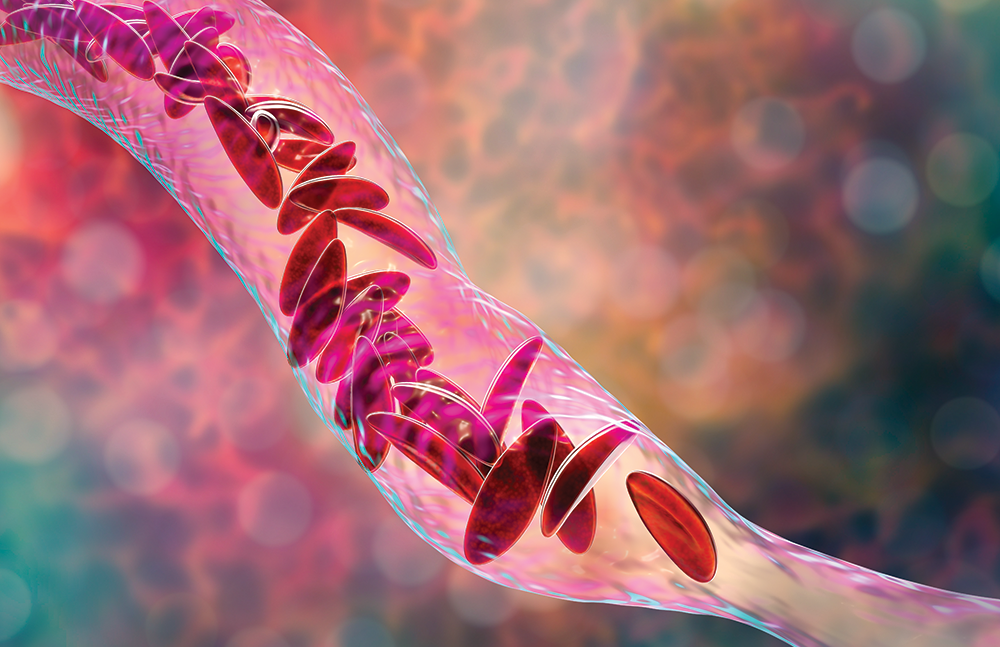
SCD is a group of inherited red blood cell disorders. Whereas healthy red blood cells are round and flexible and move around the body easily, a patient with SCD has red blood cells that are c-shaped, like a farm tool called a sickle. These cells are inflexible and do not move easily—and, as a result, they can become stuck and clog the blood flow. SCD, a genetic condition present at birth, is most typically found during routine newborn screening tests via bloodwork. Every state in the United States as well as the US territories require that all babies be tested for SCD during newborn screenings. This early diagnosis is critical, as SCD is a lifelong disease, even though a blood and bone marrow transplant can help manage complications.
It’s estimated that 100,000 Americans are living with SCD. The risk is significantly higher for African Americans; SCD occurs in approximately 1 of every 365 Black or African American births, and roughly 1 in 13 Black or African American babies is born with sickle cell trait (SCT), meaning they have a mutated copy of the HBB gene (which is responsible for making beta-globin, a component of red blood cells). People living with SCT typically don’t have any symptoms of SCD but can pass the disease on if the other parent is also a carrier.
There are a wide number of complications that may result from SCD, largely depending upon where sickle cells are flowing in the body. The disease can lead to heart problems, including coronary heart disease and pulmonary hypertension; eye problems, as the sickle cells can injure blood vessels in the eye—most often the retina; and stroke or “silent brain injury,” the latter of which is damage to the brain in the absence of outward signs of a stroke. Along with many other potential complications, SCD can also cause chronic pain.
The pain associated with SCD is greatly variable, Gupta says. It can be experienced in different parts of the body for different reasons, including occlusion of blood vessels, leg ulcers, or avascular necrosis. Some patients experience pain briefly, and others are in pain for weeks at a time. Pain may be experienced in the chest, abdomen, joints, or even the bones. Gupta adds that temperature—such as cold—can be a trigger for pain, as can wind speed.
The variability in pain creates a need for larger studies with more participants in order to be able to gain a better picture of how cannabis can fully benefit people with chronic pain, Gupta adds. But the findings from their research—published in JAMA Network Open—are promising.
The double-blind, placebo-controlled trial utilized gold-standard methods to assess the potential of cannabis to alleviate pain. Twenty-three patients with SCD-related pain participated, inhaling vaporized cannabis or a vaporized placebo during two five-day inpatient sessions that were separated by at least 30 days. This allowed them to act as their own control group. The cannabis contained equal parts THC and CBD.
As participants’ pain levels were assessed throughout the study period, the effectiveness of the cannabis appeared to increase over time, Gupta says, adding that although pain levels were typically lower in patients given cannabis than in those who inhaled the placebo, the difference wasn’t statistically significant.
“When observing the patients given cannabis, their sleep, their mood, their overall well-being all improved,” she says. “Their mood improved significantly, and overall parameters interfering with pain improved. However, we need a study with a much larger number of patients to be able to show that statistical significance for the scientific community.”
Gupta is quick to point out that vaporization, as used in this study, isn’t the same as smoking or vaping—a distinction of critical importance for SCD patients. “When we vaporize the cannabis, the vapors are filtered and collected and no particulate matter is going into the lungs,” she explains. “With this method, we could administer the exact amount that we wanted.”
Because many SCD patients already have lung complications and damage, Gupta says, it was crucial that no particulate matter entered their lungs. Similarly, Gupta says, any oral form of cannabis would have to go into the liver and be metabolized in large amounts, something they were also looking to avoid, as many SCD patients also have compromised liver systems.
“One of our criteria was to find a way to control pain by sending treatment to the nervous system without involving other organs,” Gupta explains. “Currently, the main treatment is opioids, but that always comes with the fear of addiction as well as a number of unwanted side effects.” The opioid epidemic, she adds, has also created a social stigma around the use of this medication—and even made it challenging for some patients to get the treatment they need.
“Even those [SCD] patients who are using opioids appropriately have a stigma attached because of the misuse of opioids outside of the SCD population,” she says. “These are patients who are in a lot of pain and need solutions, but the stigma associated with opioid use has prevented some patients from getting them.”
Though the research on cannabis is promising, Gupta says patients taking it on their own must be cautious. Given the fact that many SCD patients already have compromised organ systems, ensuring that they receive cannabis that’s truly pure—and safe—is vitally important.
“It’s already been found that, at times, patients who have bought cannabis on their own were not taking something pure but instead had been given something harmful and that led to serious complications,” Gupta says. “Going forward, it will be incredibly important that SCD patients do not use cannabis unless it has been proven to be pure. We understand that patients in pain may not want to drive 40 miles to a dispensary when they can get something delivered to their doorstep that is claiming to be cannabis. But there’s a significant safety issue for this vulnerable patient population.” Physicians who recommend cannabis can help direct chronic pain patients to safe and reliable sources, Gupta says.
“Research like ours continues to highlight the importance that pain patients receive cannabis from a reliable source and don’t deviate from that plan on their own,” she says. “As more research continues to come out on the ability of cannabis to alleviate pain, it will be more important than ever that patients are directed to safe and reliable dispensaries.”
— Lindsey Getz is an award-winning freelance writer in Royersford, Pennsylvania.
